HOW IS CERVICAL CANCER PREVENTED?
The most common form of Cervical Cancer starts with precancerous changes, there are 2 ways to curb the development. The first way is to prevent the precancerous (early stage of cancer) and the second is to find and treat pre-cancers before they become cancerous.
HOW TO PREVENT PRE-CANCERS
Avoid being exposed to HPV: You can prevent most pre-cancers of the cervix by avoiding exposure to HPV. Certain types of sexual behavior increase a woman’s risk of getting HPV infection such as:
- Having sex at an early stage
- Having many sexual partners
- Having a partner who has many sex partners
- Having sex with uncircumcised males.
Delay sex: Waiting to have sex until you are older can help you avoid HPV. It also helps to limit your number of sexual partners and to avoid having sex with someone who has many sexual partners. Someone can have HPV for years yet have no symptoms. Someone can also have the virus and pass it on without knowing it.
Use condoms: Condoms provide some protection against HPV. When condoms are used correctly they can lower the HPV infection rate by about 70%. Condoms cannot protect completely because they don’t cover every possible HPV-infected area such as skin of the genital or anal area.
Abstinence: Avoiding sex completely.
Don’t smoke: Not smoking is another important way to reduce the risk of cervical pre-cancer and cancer.
Get vaccinated: Vaccines have been developed that can protect women from HPV infections. So far, vaccines that protects women against HPV types 6, 11, 16 and 18 have been produced. They are known as Gardasil® and Cervarix®.


Vaccination against Human Papilloma Virus infections (HPVinfections)
HPV vaccines (Gardasil and Cervarix) are prophylactic vaccines, meaning that it is designed to prevent the initial establishment of HPV infections. For maximum efficacy, it is recommended that girls receive the vaccine prior to becoming sexually active. HPV vaccines will not block infection with all of the HPV types that can cause cervical cancer; therefore, the vaccine should not be considered a substitute for routine screening. The vaccine is administered in three injections over the course of six months. The second injection is given two months after the first one, and the third injection is administered four months after the second shot (schedule:0,2,6 months). All three doses should be given within a period of one year.
The primary vaccination series consists of 3 separate 0.5ml doses; the need for a booster has not been established. The vaccine is administered by intramuscular injection. The preferred site is the deltoid area of the upper arm.
SIDE EFFECTS
These vaccines contain no live virus and so cannot cause infections with HPV or any of the diseases HPV can cause.
These vaccines (Cervarix and Gardasil) are not interchangeable. The three-dose vaccine course should be completed with the same brand of HPV vaccine, for example, if the first injection is Gardasil, the next two injections to complete the vaccine course should be with Gardasil.
Vaccines and their possible side effects can affect individuals in different ways.
The following side effects that are known to be associated with these vaccines include:
General disorders and administration site conditions:
Very common: pyrexia.
Very common at the injection site: erythema, pain, swelling.
Common at the injection site: bruising, pruritus.
General disorders: Asthenia, fatigue, malaise.
Respiratory thoracic and mediastinal disorder:
Very rare: bronchospasm.
Skin subcutaneous tissue disorder:
Rare: urticaria.
Blood lymphatic system disorder:
Lymphadenopathy.
Immune system disorders:
Hypersensitivity reactions including: anaphylactic\ anaphylactoid reactions.
Nervous system disorders:
Guillain-barre syndrome, dizziness, headache, syncope.
Gastrointestinal disorders:
Nausea, vomiting.
Musculoskeletal and connective tissue disorders:
Arthralgia, myalgia.
The side effects listed above may not include all of the side effects reported by the vaccine’s manufacturer.
FINDING PRE-CANCEROUS CHANGES
Another way to prevent Cervix Cancer is to have testing (screening) to find pre-cancers before they turn into invasive cancer (metastasis). If a pre-cancer is found and treated, it can help stop Cervical Cancer before it really starts. Most invasive Cervical Cancers are found in women who have not had regular tests.
Sali Hoe Cervical Cancer Screening and Vaccination Center will be using an automated screening machine not Pap smear test. (automated machine is a computer image analysis system for cervical cancer screening).
Photo
An automated cervical cancer (HPV infections) screening machine
PAP TEST
This screening test (Pap test) is not a diagnostic test (manual screening). An abnormal screening result means that patient will need to have other tests (simple and advanced diagnostic tests) to find out if cancer or pre-cancerous change is actually present.
Cytology is a branch of science that deals with the structure and function of cells. It is also a manual test done to diagnose cancer by looking at cells under the microscope.
Pap test or Pap smear is a procedure used to collect cells from the cervix for cervical cytology testing. There are 2 main ways to prepare samples so that they can be examined under a microscope in the laboratory.
- CONVENTIONAL CYTOLOGY
- LIQUID BASE CYTOLOGY


Cytology Specimen
For about 50 years, all cervical cytology samples were handled this way and are relatively inexpensive but it does have some disadvantages. One of the problems with conventional cytology is that the cells smeared onto the slides are sometimes piled up on each other making it difficult for Pathologist to see abnormal cells through the microscope and most time health professional reports patients result as normal.
HOW PAP TEST IS REPORTED?
The most widely used system for describing Pap test results is The Bethesda System (TBS). This system was developed in 1988, and has been revised twice in 1991 and 2001.
2001 version (TBS) categories:
* Negative for intraepithelial lesion or malignancy
* Epithelial cell abnormalities
* Other malignant neoplasms
Negative for intraepithelial lesion: means there are no signs of cancer or precancerous changes. Specimens in this category appear entirely normal. Others may have findings that are unrelated to cervical cancer; such as signs of infections (with yeast, herpes or trichomonas). Some cases may also show “reactive cellular changes”.
Epithelial cell abnormalities: The second category epithelial cell abnormalities, means that the cells of the lining layer of the cervix show changes that might be cancer or a precancerous condition.
Further divided into 4 categories
- Atypical Squamous Cells (ASCs); these are further divided into ASC – U and ASC- H.
- Low-grade Squamous Intraepithelial Lesions (SILs)
- High-grade Squamous Intraepithelial Lesions (SILs)
- Squamous cell carcinoma
1 Atypical Squamous Cells: This category includes atypical squamous cells of uncertain significance (ASC – US). This term is used when there are cells that look abnormal, but it is not possible to tell by looking at the cells under a microscope whether the cause is infection, irritation or precancerous. Most of the time, cells labeled ASC-US are not pre-cancer. Some doctors will recommend repeating the Pap test after several months. Some doctors use the HPV DNA test to help them decide the best plan. If a woman with ASC –US is infected with high-risk type of HPV, doctors are more inclined to do a colposcopy. If a high grade SIL is suspected, it is called ASC – H and colposcopy is recommended.
- Squamous intraepithelial Lesions (SILs): These abnormalities are divided into low grade SIL and High grade SILs. High grade SILs are more likely than low-grade SILs to go away without treatment. High-grade SILs are also more likely to develop into cancer if they are not treated. Treatment can cure all SILs and prevent true cancer from developing. The need for this is based on the results of the colposcopy.
- Squamous Cell Carcinoma: This result means that the woman is likely to have an invasive squamous cell cancer. Further testing will be done to be sure of the diagnosis before treatment can be planned.
* ADENOCARCINOMA: Cancers of the glandular cells are reported as adenocarcinoma. The pathologist examining the cells can suggest whether the adenocarcinoma started in the endocervix, in uterus (endometrium) or elsewhere in the body.
* ATYPICAL GLANDULAR CELLS: When the glandular cells do not look normal but have features that do not permit a clear decision as to whether they are cancerous, it is known as typical glandular cells. The patient will have more testing if a cervical cytology result shows atypical glandular cells. (DETAILED GUIDE: CERVICAL CANCER; AMERICAN CANCER SOCIETY).
SIMPLE DIAGNOSTIC TEST FOR CERVICAL CANCER
Several types of biopsies are used to diagnose precancer and cervical cancer. Following an abnormal pap test, a colposcopy is performed.
Colposcopy: If the symptoms suggest or the screening result shows abnormal cells patient will need to have a test called colposcopy.
Colposcope is an instrument with magnifying lenses (like binoculars) that will enable the doctor see the surface of the cervix closely and clearly. Then doctor may treat the cervix with a weak solution of Acetic Acid (similar to vinegar) to make abnormal areas easier to see.
Method: In this procedure the patient will lie on the examination table. A sterilize speculum will be placed in the vagina to help the doctor see the cervix. Colposcopy is not painful and has no side effects and can be done safely even if you are pregnant. If an abnormal area is seen on the cervix a biopsy will be done. For a biopsy, a small piece of tissue is removed from the area that looks abnormal. The sample is sent to the pathologist to look at under a microscope. A biopsy is the only way to tell for certain whether an abnormal area is precancerous or invasive cancer.
A doctor examining a patient

CERVICAL BIOPSIES
Several types of biopsies are used to diagnose cervical pre-cancers and cancers.
- Colposcope biopsy: Examines the cervix with a colposcope to find the abnormal areas. Using forceps, a small section about (1/8 inch) of the abnormal area on the surface of the cervix is removed. The biopsy procedure may cause mild cramping or brief pain, and may bleed slightly afterward. A local anesthetic is sometimes used to numb the cervix before the biopsy (exocervix).
 Cervical biopsy
Cervical biopsy
- Endocervical curettage (endocervical scraping): The colposcope does not help the doctor see into the endocervix. The endocervix will have to be scraped to see if it is affected by pre-cancer or cancer. A narrow instrument called curette is inserted into the endocervical canal (the passage between the outer part of the cervix and the inner part of the uterus). Some of the tissue that is lining the endocervical canal is removed by scrapping with the curette. This tissue sample is sent to the laboratory for examination. Patient may also feel cramps and slight bleeding. Anesthetic is sometime used to numb the cervix.
- Cone Biopsy: In this procedure, also known as conization, the doctor removes a cone-shaped piece of tissue from the cervix. The base of the cone is formed by the exocervix and the point or apex of the cone form the endocervcal canal. THE TRANSFORMATION ZONE (the border between the exocervix and endocervix) is contained within the cone. The cone biopsy can also be used as a treatment to completely remove many pre cancers. Having a cone biopsy will not keep most women from getting pregnant, but if a large amount of tissue has been removed, women may have a higher risk of giving birth prematurely.
TWO METHODS COMMONLY USED FOR CONE BIOPSY
- LEEP (Loop Electrosurgical Excision Procedure)
- COLD KNIFE CONE BIOPSY
- LEEP also known as large loop excision of the transformation zone (LLETZ), in this method, the tissue is removed with a thin wire loop that is heated by electrical current and acts as a scalpel. For this procedure a local anesthetic is used and it can be done in the doctor’s office. It takes only about 10 minutes. You may have mild cramping during and after the procedure, and mild to moderate bleeding may persist for several weeks.
- Cold knife Cone biopsy: This method uses a surgical scalpel or a LASER instead of a heated wire to remove tissue. It requires general anesthesia (you are asleep during the operation) and done in a hospital, but no overnight stay is needed.
After the procedure, cramping and some bleeding may last for a few weeks.
How biopsy results are reported: The terms for reporting biopsy results are slightly different from The Bethesda system (TBS). They are illustrated below:
Biopsy results – Cervical intraepithelial neoplasia (CIN) or rarely called dysplasia.

The cervix
TBS (Pap test results) – squamous intraepithelial lesion (SIL)
OTHER OPTIONS OF REMOVING ABNORMAL CELLS
- Cryosurgery/laser surgery: During cryosurgery, the doctor uses a metal probe cooled with liquid nitrogen to kill the abnormal cell by freezing them.
Laser surgery: The doctors use a focused beam of high-energy light to vaporize (burn off) the abnormal cells or tissues. This is done through the vagina with local anesthesia. Both options can be done in a doctor’s office or clinic. After treatment, you may have a lot of watery brown discharge for few weeks. A follow up exams is required to make sure the abnormality does not reoccur. If it does the treatment can be repeated.
HPV DNA TEST
Doctors can now test for the types of HPV that are likely to cause cervical cancer (high-risk types) by looking for pieces of their DNA in cervical cells.
HPV DNA test is used in combination with the Pap test to screen for cervical cancer in woman over 30 years.
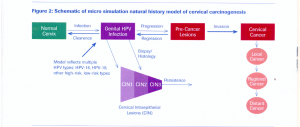
The HPV DNA test is also used in women of any age who have slightly abnormal Pap test results, to find out if they might need more testing or treatment. See diagram below:

